This has nothing to do with tampons in the heart ok! Just an FYI.
When blood or fluid accumulate in the sac which surrounds the heart it exerts pressure against the heart, making it harder for the heart to pump. As you can imagine, if the ventricles cannot fill fully or contract effectively then cardiac output decreases. Decrease cardiac output is not good news!
So how do you know if someone has this?
Well the symptoms are nothing unusual: chest pain, restlessness, quick shallow breathing, palpitations, pallor, tachycardia, weak peripheral pulses, pulsus paradoxical, distended neck veins, low BP… (do these all sound a little familiar? MI anyone?) Well causes of cardiac tamponade can be MI, Dissecting aortic aneurysm (thoracic), end-stage lung cancer, heart surgery, Pericarditis caused by bacterial or viral infections, or direct wounds to the heart.
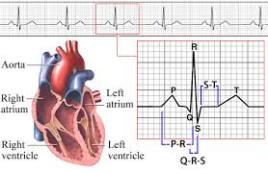
How do we diagnose? Echocardiogram is the usual diagnostic tool, but MRI, CT, CXR or EKG can also highlight or confirm this.
This is an emergency! The fluid must be drained to reduce damage to the myocardium and reestablish cardiac output.
Pericardiocentesis is a procedure that uses a needle to remove fluid from the pericardial sac, the tissue that surrounds the heart. The patient will be hyperoxygenated, given fluids to maintain blood pressure. It is important to note that a pericardiocentesis may have to be repeated because cardiac tamponade can return. With fast treatment the outcome is usual good, without treatment death is immanent.

A pericardial draining tube may be placed during surgery to keep in place postop. The drainage will be measured every shift and documentation on the color, amount and consistency is very important! The tube will usually be removed slowly over the postop recovery weeks at the discretion of the cardiologist.